Asha is Hindi for hope. That’s what these women – one million strong – have brought to Covid-ravaged India
“Here they come again…,” the woman in the green saree mutters under her breath as two women in radiant pink sarees walk towards her.
“I won’t. I won’t. I won’t take the vaccine,” Masanamma shouts at them. “I’ve told you this before!”
“But why?” asks Mahadevi, one of the pink sari-clad women, with a knowing smile.
“I’ll die if I don’t take the shot. And, I’ll die if I take one,” Masanamma says. “So, I’ve decided to die without it,” she declares, with an air of finality.
Other women, who have gathered around a harvest of millet drying on a concrete floor, nod approvingly at Masanamma.
It’s an early July morning, and this back-and-forth is not unusual for Mahadevi, who is conducting a door-to-door Covid-19 vaccination awareness drive in Muthugada Gadde, a hamlet of the indigenous Soliga tribe in the Biligiri Rangana Hills, on the edge of a tiger reserve in the southern Indian state of Karnataka.
Mahadevi is an Accredited Social Health Activist (ASHA) — a rural, frontline volunteer. India’s rural healthcare system runs on a million of these all-women ASHA workers, who in this pandemic are also responsible for disseminating vaccine messages and bringing people to vaccine centres.

Usually one ASHA is assigned for a population of 1,000 people. In the tribal areas of the Biligiri Rangana Hills where settlements are scattered across forests and hills, there is one ASHA for a population of 400, with each ASHA responsible for two or three settlements.
For the vaccine drive, four ASHA workers have teamed up with an Auxiliary Nurse Midwife (ANM), and two health department officials to cover 10 settlements with a population of 2,400.
In private conversation, 26-year-old Mahadevi comes across as a little reticent, even shy. But during the vaccine drive, when ambushed with questions on vaccine safety, she seems emboldened and answers every question in her native Soliga language.
“The vaccine won’t kill you,” she tries to assure Masanamma.
“I’m perfectly healthy now; why should I risk it?” shoots back Masanamma. “Ketegowda (a neighbour) fell sick after the injection. There was nothing wrong with him but for the vaccine.”
“I got two shots. I’m fine, standing here in front of you. Why do you think it will kill you?” asks Mahadevi. “I’ll come again. I’ll keep coming till you take the vaccine.”

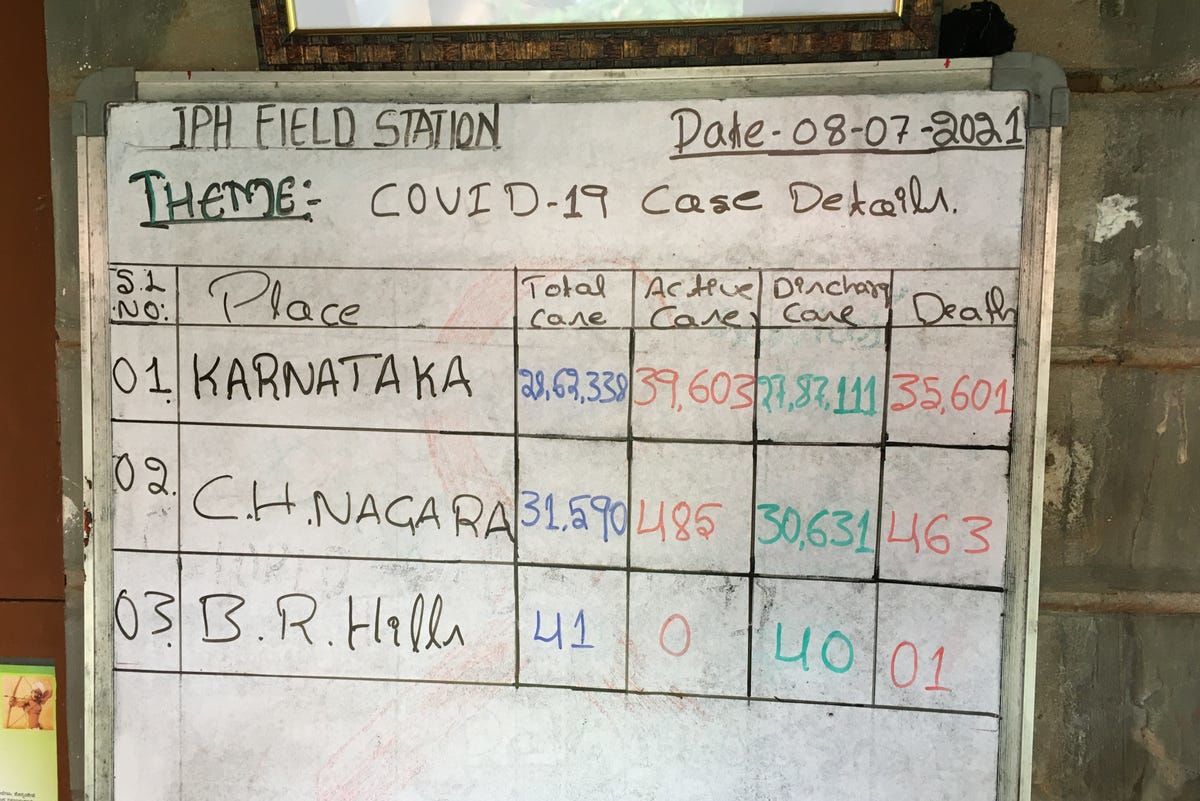
India was ravaged by a second wave of Covid-19 this year, with both cases and deaths peaking in May 2021. By mid-July, more than 31 million cases and 414,000 deaths were officially recorded. But many reports estimate that the true number of deaths due to Covid-19 in India may be anywhere between 600,000 and 4.2 million.
So far, Indian health workers have administered more than 400 million doses of the vaccine but assuming everyone needs two doses, that means less than 15 per cent of the population is fully vaccinated. One reason for the slow rate of vaccination is lack of supply. Another challenge has been vaccine hesitancy among some groups, compounded by misinformation.
WhatsApp users are spreading rumours about impotency, blood clots and death as side effects of Covid vaccination. One story about a person acquiring magnetic power post vaccination was widely shared. Others spoke about possible risk of infertility and the need to avoid vaccination during menstruation. Several anti-vax groups are active too, with doctored videos, fake interviews and dubious documentaries.
In Biligiri Rangana Hills, the Soliga community’s apprehension about the vaccine turned to fear after one person died post-vaccination in May. Health workers and community leaders attributed the death to a pre-existing condition, but the community refused to participate in the government’s vaccination drive.
Over the day, Mahadevi hears many justifications for avoiding the jab. One man tells her: “We live in the forest, we don’t venture out, and we’re isolated. We eat healthy and breathe fresh air. How will we get Covid?” A woman says: “I’ll get Covid from you because you go around several villages. You stay away from me. You need a vaccine because you roam around villages; I don’t.”
On one day in May, the health team arrived at a settlement in a jeep. At the sound of the vehicle, people ran into the forest. Later, they blocked the road with thorny bushes and rocks to keep the vaccine team away, opening it only after a month, when the team convinced the panchayat (elected village council) leaders that they needed access for non-vaccination services such as deliveries.
“The hesitancy is due to historical exclusion of this community. Trust had not been built earlier,” says Dr Prashanth Nuggehalli Srinivas, a local doctor and a public health researcher with the Institute of Public Health, an academic institution.
“People are questioning why the government is taking sudden interest in saving their lives when their pleas for electricity and piped water have been ignored for decades.”

To try to rebuild trust, ASHA workers are going door-to-door to convince Soligas to get vaccinated. They address doubts and show photos and videos of people from the same community who are healthy post vaccination.
On June 17, they organised a day-long meeting at a community hall. At least 35 leaders from 10-12 Soliga hamlets attended. The next day, when a state cabinet minister visited the vaccine centre, one of the Soliga leaders from the village that blocked the road, turned up to be vaccinated. Six other people, including a female teacher, also took the jab.
After that, more people started coming in, says Mahadevi. “The numbers are small but the trickle has started. Now, we are holding similar meetings in other settlements.”
Another major hindrance in the vaccination programme is the long distances people have to travel —up to 25 kilometres— to health centres. Following requests from community organisations, the government has organised vaccine camps in small tribal villages.
June witnessed a surge in vaccinations in these areas, with 51 people getting vaccinated on June 21— the highest number administered in a single day. Bucking the trend seen in the rest of the country, more women are getting vaccinated than men.
Everybody can see what wonders health workers from indigenous communities have done in terms of driving the numbers up, a lesson for the vaccine rollout to other marginalised groups, says C Made Gowda, secretary of a community-based organisation, and the first Soliga to get a PhD degree.
For instance, Yerakana Gadde hamlet, Mahadevi’s home village, is witnessing a steady rise in vaccinations.
It’s not a coincidence, says Gowda. “If the ASHA worker is from the same community, access and trust is higher. We’re now pushing the district administration to hire more ASHAs from the indigenous community.”

The ASHA system has worked for a number of reasons. ASHAs have direct access to every household and assist women with reproductive and maternal healthcare. They speak local languages and are therefore the last line of defence against misinformation.
With most of them fully vaccinated in the government’s effort to safeguard frontline workers, they are now the ambassadors of the safe vaccine message.
ASHA is a crucial connection between the hospital and a village with no doctor, says Ashish Ranjan, who runs an NGO in the eastern state of Bihar. “She works for the government and also has society’s trust since she is one among us. A big village has ten to fifteen ASHAs, making their presence ubiquitous.”
These semi-educated women, often from disadvantaged sections of the society, have reached out to people on the margins— indigenous peoples, oppressed castes, and women in rural India.
A similar strategy of community health workers’ involvement should work for vaccination drives in other countries, says Dr Srinivas of the Institute of Public Health.
“Many African countries have a community health workers system; Ethiopia has a system similar to ASHA. They must involve them if they are looking to vaccinate widely. But, for a successful drive, these workers need to be better resourced and better protected,” he says.
In the eastern state of Bihar, with some of the worst health indicators in the country, ASHA women are at the forefront of the effort to bring vaccinations to oppressed castes.
Misa Bharti, a 28-year-old ASHA in Belsara village in Araria district, received no training from the health department on how Covid vaccines work or how to answer questions on vaccine hesitancy.
So she employed her common sense and decided to be the one asking the questions.
“Did your kids get inoculated for DPT (Diphtheria, Tetanus & Pertussis) or BCG (tuberculosis vaccine)?” she quizzed those with doubts.
“Didn’t they develop a fever after that? Does that mean the vaccine is bad for them?”
Vaccines are important for everybody’s safety, she says. “But it is crucial for Mahadalits (the most oppressed castes) most of whom migrate for work as daily wage labourers. Their exposure to other people is very high. Getting vaccinated makes their travel and work safer.”
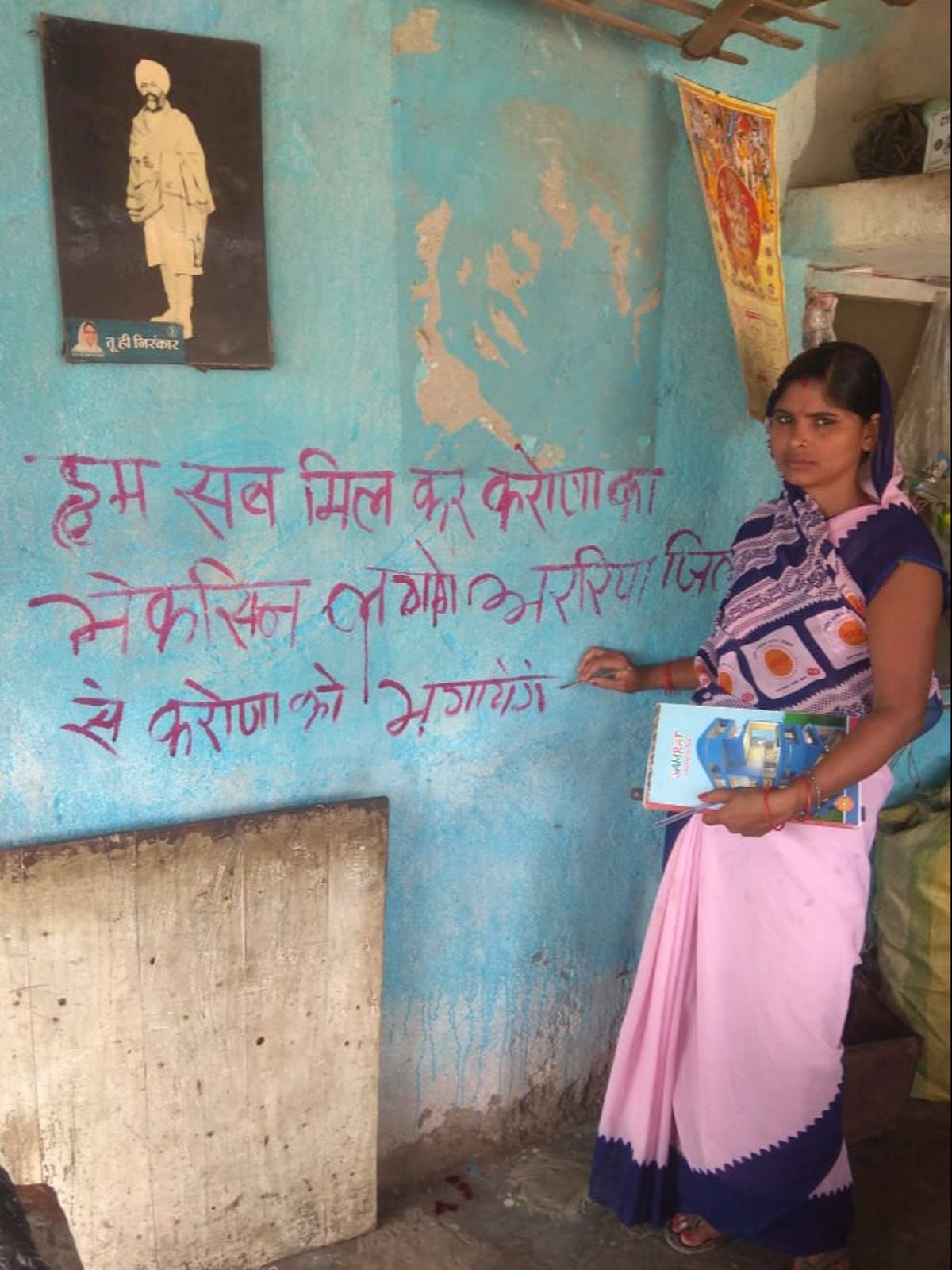
But low literacy rates (4.6 per cent overall, 1.3 per cent for women) make it harder to get the message across to this community, says Bharti. And so when small group of 25 Mahadalits came for the vaccine in mid-June, Bharti saw it as a sign of change. “Now, more and more Mahadalits are coming for the vaccine. Soon, they will all be vaccinated.”
As well as the most marginalised castes, women lag behind men in Covid vaccination across India. For every 1,000 men vaccinated, only 867 women have been given the jab.
In the northwestern state of Punjab, the gender gap is even more stark, with only 754 women vaccinated for every 1,000 men. Again, ASHA workers have come to the government’s rescue, and have proved to be the biggest driving force behind women’s vaccination.
Ranjit Kaur in Phool Khurd village in Rupnagar district is responsible for sourcing vaccines from major health centres as well as motivating and registering people to get vaccinated.
Over 70 per cent of the 1,000 people she is responsible for are now vaccinated. “Women are coming in such large numbers to get vaccinated that we’re running short of vaccines.”
“When they were hesitant, I gave them my own example for vaccine safety. They listen to me because they have known me for years. I am their neighbour. I’ve helped them get hospitalised for their deliveries.”
If not for ASHA workers, the government wouldn’t have been able to reach even half the women, especially in rural areas, she says. No outsider could go and speak to women, win their trust and convince their families about the importance of vaccination.
“The government hasn’t kept its promise of paying incentives for Covid-related work, but I’m keeping mine (as a community health worker).”

Despite their crucial role, the ASHA women’s jobs are classed as temporary and most states, including Bihar and Punjab, don’t pay them monthly wages. They are paid task-based incentives, which often work out to below the minimum daily wage set by the government of £1.72. In Karnataka, Mahadevi gets paid only 4,000 rupees (£39) per month but hasn’t received her salary since April.
Several states have failed to pay their wages during the pandemic while forcing ASHAs to work without adequate protective gear, leading to loss of lives. In protest, ASHAs have held countrywide strikes several times during the pandemic.

In the Biligiri Rangana Hills, Mahadevi has wound up her rounds in two settlements and is walking ahead of her team to another village. She spots a group of men sitting on the roadside, and one of them is Ketegowda, whose sickness the villagers cited as a reason for their fear of the vaccine.
“I did fall sick,” he says. “But that was a month after getting the second dose. And, I’m perfectly fine now.” Several people have asked him about it. “I told them I was absolutely fine. And that my sickness wasn’t related to the vaccine. Still, some believe it was.”
“Next time, I’ll ask Ketegowda to come with me on village rounds,” Mahadevi laughs.
A few yards down the road, a woman comes running towards her. “When am I getting the vaccine?” she asks.
She is from a group of workers who are digging a pond. They surround Mahadevi. “Has the new stock come?” asks one of them. “You’ve been making me wait for two weeks,” says another woman. “How many times do I need to call you for a vaccine?”
Mahadevi’s centre has had no vaccine stock since the start of the month, reflecting a lack of supply across the country.
“Now, it seems like there’s going to be a quarrel over vaccines,” remarks a man.
Mahadevi smiles at this. A grey hornbill flies overhead before settling on a tree.
“From now on, it’s the shortage of vaccine supply that’s going to be the problem here,” Mahadevi says. “Not hesitancy.”















